What is keratoconus?
Keratoconus is a progressive disease that causes thinning and reshaping of the cornea, the front part of your eye.
In a healthy eye, the cornea is clear and dome-shaped. When keratoconus develops, the cornea becomes thin and begins to bulge like a cone. This distorted shape causes blurry and distorted vision as the light that enters the eye can no longer properly focus onto the retina.
Keratoconus usually causes mild to severe astigmatism, and nearsightedness, making reading and driving difficult. Keratoconus can also cause corneal swelling and scarring, and even vision loss.
What are the symptoms of keratoconus?
Keratoconus is often diagnosed among teens and young adults, and progresses for up to 20 years until it plateaus. Symptoms usually start out mild and become progressively worse over time— usually over a decade or two. In some cases, keratoconus symptoms progress rapidly.
Keratoconus frequently affects both eyes, and can lead to different optical prescriptions between the two eyes.
Symptoms of keratoconus may change over time, and can differ in each eye.
In its early stages, symptoms are generally mild, and may include:
- Blurred vision
- Distorted vision, straight lines appear wavy
- Light sensitivity
- Glare
- Eye swelling or redness
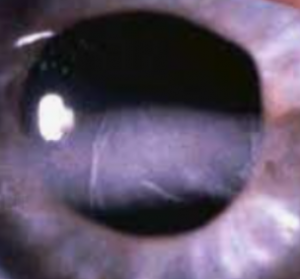
If keratoconus causes swelling, it will also cause the scarring over the corneal tissue— causing the cornea to become opaque and more difficult to see through. With corneal scarring, vision therefore becomes more blurry and distorted.
In its later stages, symptoms generally include:
- Increased vision distortions and blurred vision
- Increased nearsightedness or astigmatism
- Contact lens discomfort
Caution: Avoid rubbing your eyes. Rubbing your eyes can cause damage to the already thin corneal tissue, and result in worsening symptoms. Speak to your eye doctor about eye drops to control any allergies that may be causing your itchy eyes.
If you suspect you have an eye condition, contact an eye doctor near you, who can diagnose and treat the condition.
SEE RELATED: Keratoconus Treatment: Corneal Cross-linking
What causes keratoconus?
While the exact cause of keratoconus is uncertain, the following factors are most frequently associated with the development of this condition.
- Genetics
- Eye trauma
- Eye allergies
- Excessive eye rubbing
- Other eye diseases
- Down syndrome
- Osteogenesis imperfecta
- Addison’s disease
- Leber’s congenital amaurosis
- Ehlers-Danlos Syndrome
How is keratoconus diagnosed?
Keratoconus is diagnosed during a comprehensive eye exam:
Corneal examination. Your eye doctor will closely examine your corneal health, and evaluate its shape and curvature.
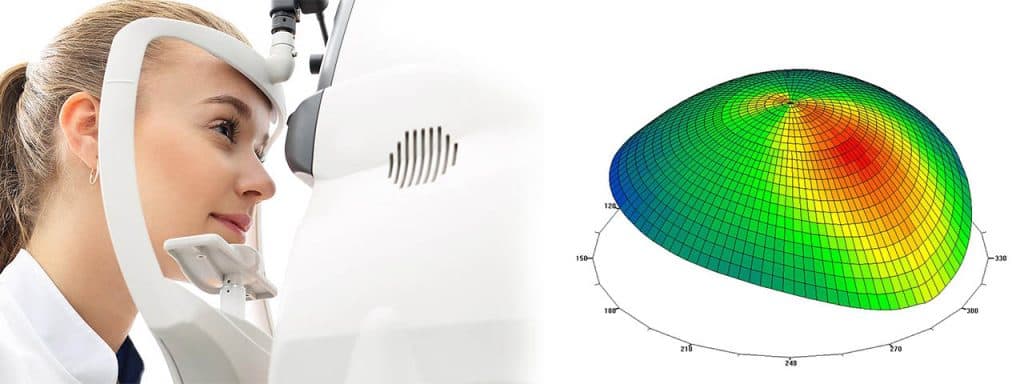
Corneal mapping (topography). This is a non-invasive diagnostic tool that provides 3-D images of the cornea. The images provide details about the cornea’s shape and curvature, and enable detection of irregular conditions.
Corneal mapping is used to detect certain corneal diseases, abrasions, deformities, and irregular astigmatisms. Corneal mapping is also used to monitor and treat ocular conditions, plan eye surgery, and fit contact lenses.
The diagnostic test involves sitting in front of an instrument called a Corneal Topographer, which sometimes appears as a lighted “bowl”, and resting your head against a bar. After your data is collected, a 3D color-coded image of your corneal shape is generated, using different colors to differentiate elevations.
How is keratoconus treated?
There are a few different ways to treat keratoconus. Your eye doctor will recommend the most effective treatment plan based on your presenting symptoms.
1. Eyeglasses and contact lenses
In its early stages, eyeglasses or soft contact lenses can correct any distorted or blurred vision.
As the disease progresses, rigid gas permeable contact lenses may be required for adequate correction.
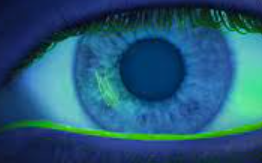
The most effective contact lenses for keratoconus are Scleral contact lenses.
2. Corneal cross-linking
Corneal cross-linking is an in-office procedure that strengthens the cornea by creating new bonds between the collagen fibers in your eye. These new bonds help to stiffen the cornea, to support its shape and provide extra resistance to the effects of worsening keratoconus.
During the procedure, the epithelium, the front layer of the cornea, is either loosened (epi-on) or completely removed (epi-off), and an eye drop of liquid riboflavin (vitamin B2) is applied to the surface of the eye.
After the liquid riboflavin eye drops have been inserted, ultraviolet light (UV) is then administered to the eye at varying levels of time and intensity, and is absorbed by the cornea. The UV light functions to stabilize the cornea and slow the progression of disease.
The epi-off procedure is 95 percent effective in stopping the progression of keratoconus. The epi-on procedure is also effective, though the data on its long term efficacy is less known, as epi-off is more commonly performed.
When corneal cross-linking is used in the early stages of keratoconus, it can prevent vision loss even before corrective lenses are needed. It is the only treatment method that can stop keratoconus from worsening and reduce your chances for a corneal transplant later on in life.
3. Intacs surgery
Intacs are thin plastic, semi-circular rings that are surgically implanted into the middle layer of the cornea to flatten cornea. The intacs hold the shape of the cornea and eliminate any abnormalities caused by keratoconus.
This procedure typically improves vision to the point that eyeglasses or contact lenses are no longer needed. In severe cases, corrective eyewear may still be required.
4. Corneal transplant
In advanced keratoconus, a corneal transplant may be necessary to replace the damaged cornea with a new one. This surgery is successful in about 90 percent of people, though most patients will still require eyeglasses or contact lenses even after the transplant.
LEARN MORE: Guide to Corneal Conditions
If you notice any changes to your vision, it is important to schedule an eye exam as soon as possible.
An early diagnosis of keratoconus can facilitate optimal treatment results, providing you the best chance of maintaining your clear vision and corneal health.