What is the cornea?
The cornea is the clear, protective outer layer of the eye. It acts as a barrier and filter— protecting our eyes from both harmful particles, and the sun’s ultraviolet rays.
The cornea also plays an essential role in vision.
As light enters the eye, it is refracted, or bent, according to the shape of the cornea. The curvature, or shape of the cornea, determines the eye’s focusing abilities for both near and distant objects.
The cornea consists of five layers:
- Epithelium:
- Most superficial layer of the cornea
- Prevents harmful particles from entering the eye
- Absorbs oxygen and nutrients from the tears
- Bowman’s layer:
- Maintains corneal shape
-
-
- Stroma:
- Thickest layer of the cornea located behind the epithelium
- Made up mostly of water and proteins that give it an elastic but solid consistency.
- Descemet’s membrane:
- Resting layer for endothelial cells
-
- Endothelium:
- A single layer of cells located between the stroma and the aqueous humor, the clear fluid found in the front and rear chambers of the eye.
- Works as a pump, removing excess water as it is absorbed into the stroma to prevent vision problems.
What is corneal disease?
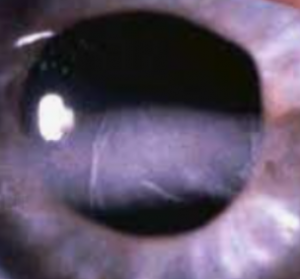
Corneal disease or infection can lead to scarring or discoloration— affecting the cornea’s normal function, and causing vision loss and even blindness.
Corneal disease that results in corneal scarring is a common cause of monocular and bilateral blindness in children and young adults.
What are the symptoms of corneal disease?
The cornea usually heals quickly after most infections or diseases have been treated.
However, when deep injury to the cornea has occurred, the healing process may take longer, sometimes resulting in a variety of symptoms, including:
- Pain
- Redness
- Tearing
- Blurry vision
- Light sensitivity
- Corneal scarring
If you experience any of these symptoms, contact an eye doctor as soon as possible.
SEE RELATED: Corneal Ulcers
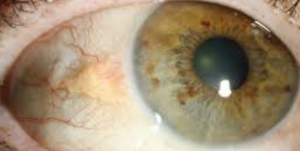
Keratitis
Infectious keratitis occurs from an infection in the cornea, or the clear layer that covers your pupil and iris. Keratitis means swelling of the cornea, and isn’t always infectious if it develops as a result of an eye infection. However, it can result from a viral, bacterial, fungal, or parasitic infection.
Approximately 25,000 Americans suffer from bacterial keratitis, annually.
Symptoms:
- Redness
- Swelling
- Eye pain
- Abnormal discharge
- Increased tear production
- Pain when opening/closing eyelids
- Blurry vision
- Reduced vision
- Light sensitivity
- Foreign body sensation
Risk factors:
- Wearing contact lenses
- Having a weak immune system
- Living in a warm or humid climate
- Using corticosteroid eye drops
- Suffering from an eye injury
Treatment:
Treatment methods will depend on the type of keratitis.
- Bacterial: Antibacterial eye drops are used for mild to moderate infections. Oral antibiotics are used to treat more severe infections. Symptoms usually subside within a few days of starting treatment.
- Fungal: Antifungal eye drops or medications are used to eliminate the fungal organisms. This type of infection can take longer to treat, sometimes weeks or months.
- Viral: There is no treatment for a viral infection— it usually has to run its course. In some cases, antiviral eye drops or oral medications will be prescribed to help stop the infection. These treatments can take anywhere between a few days to a week to relieve symptoms. However, even with treatment, symptoms may reoccur.
Ocular herpes (herpes of the eye)
Ocular herpes, most commonly called eye herpes, develops when the eye is infected by the herpes simplex virus (HSV-1). Sometimes referred to as a ‘cold sore on the eye’, this condition is a common, recurring viral infection that causes inflammation and, if left untreated, can cause permanent scarring of the cornea.
Eye herpes is highly contagious and can be transmitted through close contact with someone who has an active virus, or through self contact and contamination from a cold sore on the lip.
The National Eye Institute (NEI) estimates:
- 400,000 Americans have had some form of eye herpes.
- 50,000 new and recurring cases occur each year.
Eye herpes can present on a wide scale of types and severity, ranging from mild to sight threatening:
Herpes keratitis: This is the most common form of eye herpes— caused by a viral corneal infection. This type of ocular herpes usually affects only the top layer (epithelium) of the cornea, and generally heals without scarring.
Stromal keratitis: This form results as the infection spreads deeper into the cornea— and can lead to scarring, and partial or total vision loss. According to NEI, about 25 percent of new and recurring cases of herpes eye infections result in stromal keratitis.
Iridocyclitis: This is a severe form of eye herpes that results from inflammation of the iris and surrounding tissues inside the eye.
Iridocyclitis: This is a type of uveitis that affects the frontal part of the eye. When the infection develops in the retina or the inside lining of the back of the eye, it is known as herpes retinitis.
Symptoms:
Symptoms can vary, depending on the type of eye herpes:
- Eye sores
- Redness
- Irritation
- Swelling
- Tearing
- Foreign body sensation
- Watery discharge
- Light sensitivity
- Recurrent eye infections
In some cases, inflammation of the cornea will cause irritation, or a sudden and severe pain in the eye, and cloudy or blurry vision.
Symptoms typically present in one eye, though can sometimes affect the other eye as well.
Risk factors:
While the exact cause of an eye herpes infection remains unknown, the following factors have been shown to lead to an increased risk.
- Fever
- Trauma
- Surgical or dental procedures
Additionally, according to the NEI:
Eye herpes has about a 50 percent chance of recurring— from several weeks or several years following the initial infection.
Treatment:
There is currently no cure for eye herpes.
In most cases, eye herpes will heal on its own in a week or two, but if symptoms persist, there are treatments that can control the infection.
If the corneal infection is only superficial, your eye doctor will prescribe an antiviral medication in the form of an eye drop, ointment, or oral medication.
If the infection has spread into the deeper layers of the cornea, corticosteroid eye drops will be prescribed to reduce inflammation and prevent corneal scarring. These drops are typically used in combination with antiviral drops.
Depending on your specific case, your eye doctor may debride, or brush off your cornea with a cotton bud to eliminate infected cells.
In rare cases when corneal scarring occurs and steroid treatments prove to be ineffective, a corneal transplant may be required to restore vision.
Herpes zoster (shingles)
Herpes zoster, also known as shingles, can cause blisters or sores on the cornea. This infection occurs as a result of the chickenpox virus. After a bout of chickenpox, the virus remains dormant within the nerves of the body, and can travel down the nerves at a later time, infecting specific areas of the body— including the eye.
Shingles, which is a recurrence of the chickenpox virus, can occur in anyone who has been exposed to the chickenpox virus, though adults over age 65, and those with a weakened immune system, have an increased risk.
Symptoms:
- Pain
- Fever
- Corneal sores
Treatment:
In most cases, corneal lesions heal by themselves, but many times, an antiviral treatment will be prescribed to shorten the course of the disease.
In some cases, patients may develop chronic corneal inflammation from the disease. In these cases, eye drops may be prescribed for long-term use. In rare cases, corneal surgery will be recommended.
How is corneal disease diagnosed?
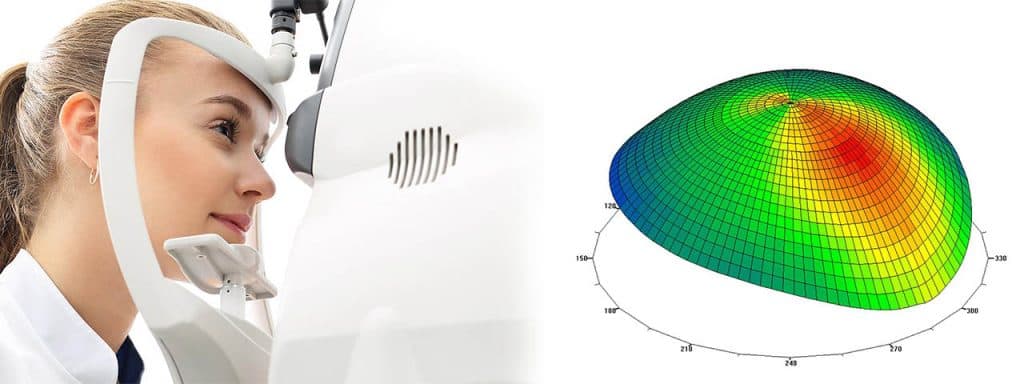
1, Corneal topography
Corneal Topography, also known as corneal mapping, is a non-invasive diagnostic tool that provides 3-D images of the cornea, or the outer layer of the eye responsible for about 70% of the eye’s focusing power. The images provide details about the cornea’s shape and curvature, and enables detection of irregular conditions.
Corneal mapping is used to detect certain corneal diseases, abrasions, deformities, and irregular astigmatisms. Corneal mapping is also used to monitor and treat ocular conditions, plan eye surgery, and fit contact lenses.
The diagnostic test involves sitting in front of a lighted “bowl” and resting your head against a bar. After your data is collected, a color coded image of the corneal shape is generated, using different colors to differentiate elevations (similar to a topographic map of the earth that displays changes in the surface of the land).
2. Slit-lamp exam
This diagnostic test examines the front of the eye by shining a beam of light shaped like a small slit on the eye. This test can be used to facilitate diagnosis of various conditions such as cataracts, macular degeneration, injuries to the cornea, and presbyopia.
Pupil dilation may be required while performing this exam.
Can corneal disease be prevented?
The best way to reduce your risk of corneal infections is by protecting your eyes from injury, and limiting physical contact with people who have contagious eye infections.
Avoid sharing eye makeup, contact lens cases, contact solutions, and eye drops— and always wash your hands with soap and warm water for at least 15 seconds after contact with an infected person.
While corneal dystrophies that result from hereditary factors cannot be prevented, vision can often be preserved through early diagnosis and treatment.
LEARN MORE: Guide to Corneal Diseases
If you think you may be experiencing symptoms of a corneal infection or disease, contact an eye doctor as soon as possible for a comprehensive eye exam.
Discuss all of your concerns of your vision or eye health with your eye doctor to enable the best possible treatment plan, and optimal results.