Diabetic retinopathy is a serious sight-threatening complication of diabetes.
This ocular disease is caused by high levels of sugar in the bloodstream and results in progressive damage to the light detecting retina responsible for sending visual signals to the brain.
- Diabetic retinopathy affects 1 in 3 people with diabetes.
- 1 in 2 people are unaware that they have diabetic retinopathy.
- 95% of people with diabetic retinopathy can avoid severe vision loss with early treatment.
Can I go blind from diabetes?
Yes, unfortunately chronic, uncontrolled diabetes can lead to blindness.
Diabetes is a condition that prevents the body from using and storing sugar properly. As a result, excessive amounts of sugar remain in the bloodstream and cause damage to the smallest blood vessels all over the body— including your eyes.
Diabetes damages the small blood vessels throughout the body, including the tiny capillaries in the retina.
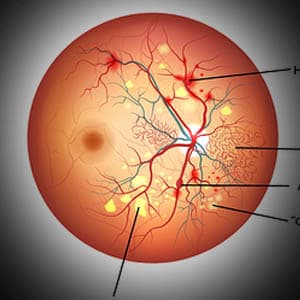
Eventually, these tiny blood vessels leak blood and other fluids into the eye, and cause the retinal tissue to swell— resulting in cloudy or blurred vision. As these blood vessels are damaged, new abnormal blood vessels are produced. These new vessels are fragile and are even more susceptible to leaking and bleeding fluid into the eye.
Diabetes also affects the focusing lens of the eyes. When blood sugar remains at high levels for long periods of time, fluid accumulates inside the focusing lens, leading to changes in the curvature of the lens and blurry vision.
However, if blood sugar levels are controlled, the lens will usually return to its normal curvature and vision will improve.
Controlling diabetes will decrease the risk of developing this sight threatening disease.
Types of diabetic retinopathy
1. Non-Proliferative Retinopathy (NPR)
Also called Background Retinopathy, this is the earliest stage of the disease. In this stage, high blood sugar concentration in the retina causes microaneurysms, in which damage to the walls of the tiny retinal capillaries occurs.
Microaneurysms eventually rupture and bleed and due the shape, are called “dot-and-blot” hemorrhages.
2. Proliferative Retinopathy (PR)
This is the more severe form of the disease. In this stage, abnormal blood vessels begin to grow in the retina.
If these new blood vessels break, it can trigger bleeding into the vitreous, gelatinous matter that fills the eye— causing retinal scarring, severe vision difficulties, and even blindness.
3. Diabetic macular edema (DME)
This is a complication of diabetic retinopathy. DME occurs when damaged blood vessels leak fluid into the macula— the part of the retina responsible for sharp central vision that allows you to see fine details.
Diabetic macular edema may cause blurry or wavy vision, blind spots, and cause colors to appear dull. These symptoms can impact reading, writing, driving, and facial recognition.
Symptoms of diabetic retinopathy
Diabetic retinopathy usually does not present symptoms in its early stages, so by the time the symptoms are noted it is essential to seek medical care.
- Blurry or cloudy vision
- Double vision
- Seeing floaters
- Increasing scotomas (dark spots)
- Near vision difficulty
- Poor night vision
SEE RELATED: 5 Tips to Prevent Diabetic Retinopathy
If you experience any of these symptoms contact an eye doctor near you who can manage your diabetic retinopathy.
How is diabetic retinopathy diagnosed?
It is crucial for people with diabetes to have comprehensive eye exams on a regular basis, to detect signs of the disease even before symptoms are noticed.
Many diabetic eye exams will include the following tests:
- Patient history to determine vision difficulties, presence of diabetes, and other general health concerns that may be present.
- Visual acuity measurements to determine the visual acuity.
- Refraction to determine if a new optical prescription is required.
- Evaluation of the ocular structures through a dilated pupil.
- Measurement of eye pressure within the eye.
Your eye doctor may also use special diagnostic tools to identify any signs of damage in your retina:
Fluorescein angiography provides a definitive diagnosis of diabetic retinopathy. During this test, a dye is injected into your arm through an IV, and is illuminated in the blood vessels of the retina. This test can detect any changes or fluid leakage in the retina, caused by diabetes.
Optical coherence tomography (OCT) scan is a non-invasive, diagnostic tool that obtains high resolution colored images of the layers of the retina. This test can accurately detect any changes to the retinal structure as well as fluid leakage into the retina.
How is diabetic retinopathy treated?
Treatment for diabetic retinopathy depends on the stage of the disease.
In the early stages of non-proliferative diabetic retinopathy, regular monitoring is crucial. Consuming a healthy diet, getting regular exercise, and controlling your blood sugar levels can all help to control the progression of the disease.
Treatment methods for diabetic retinopathy include:
1. Anti-Vascular Endothelial Growth Factor (Anti-VEGF) treatments block the protein that when present at high levels, can cause the blood vessels to leak fluid and abnormal blood vessels to grow.
Anti-VEGF medication is administered by your eye doctor through eye injections using a tiny needle. Your doctor will advise how many treatments will be necessary for treatment of your individual case.
Types of anti-VEGF medications:
- Avastin uses a drug called bevacizumab.
- Lucentis uses a drug called ranibizumab
- Eylea uses a drug called aflibercept and is generally used to treat DME.
All three medications have been proven safe and effective. Each medication works to block the growth of abnormal blood vessels in the back of the eye, but differ in the type of drug they use, as well as their cost.
2. Laser photocoagulation involves sealing the blood vessels that are leaking into the eye, thereby inhibiting abnormal blood vessel growth. A laser beam of light creates small burns in areas of the retina with abnormal blood vessels to try to seal the leaking blood vessels.
3. Pan-retinal photo-coagulation is a laser procedure on the peripheral retina used to maintain unaffected vision, by destroying tissue on the outside of the retina which is not needed for basic vision, thereby increasing blood supply to the inner portion of the retina.
4. A vitrectomy is a procedure that removes the blood that has leaked into the vitreous humor. This procedure is generally performed if all other treatments were ineffective.
Untreated diabetic retinopathy can lead to many complications, and even blindness. However, with proper treatment, and maintenance of healthy blood sugar levels, many symptoms of diabetic retinopathy can be reversed.
Risk factors for diabetic retinopathy
The longer you have had diabetes, the higher your risk of developing diabetic retinopathy.
Other factors that may increase your risk include:
- Type 1 or type 2 diabetes
- Gestational diabetes
- Poorly controlled diabetes
- Hispanic or African American decent
- High blood pressure
- High cholesterol
Prevention
Follow these recommendations to help reduce your risk of the disease, as well as control its progression.
- Take medication as prescribed
- Control blood sugar levels
- Consume a healthy diet
- Avoid excessive alcohol
- Quit smoking
- Get regular exercise
- Schedule routine eye exams
LEARN MORE: Guide to Eye Conditions
If you or a loved one has been diagnosed with diabetes, it is crucial to schedule annual comprehensive eye exams to monitor any changes in your ocular health and enable early detection of disease.
Early detection of diabetic eye changes are a key factor in both controlling and treating diabetic retinopathy.