Have you been diagnosed with macular degeneration?
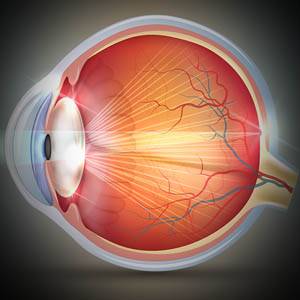
Macular degeneration, also known as age-related macular degeneration (AMD), is an ocular disease caused by deterioration of the macula, the center of the retina that controls your visual acuity.
- Macular degeneration accounts for 8.7% of blindness worldwide
- Macular degeneration is the #1 cause of low vision
What are the symptoms of AMD?
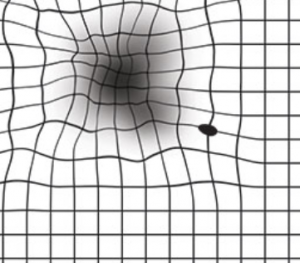
Macular degeneration causes dark “blind” spots to appear in the center of an image, or anything you are viewing, with gradual loss of central vision. The disease affects performance of visual tasks that include fine details — reading, driving, recognizing faces, using a computer, watching TV, etc.
It is crucial for AMD to be diagnosed and treated in its early stages to prevent severe vision loss and sometimes even blindness.
Early signs of AMD include:
- Blurry vision
- Cloudy vision
- Dark ‘blind’ spots
Signs of AMD in its advanced stages:
- Sudden, severe vision loss
- Larger blind spots
- Loss of central vision
Types of Macular Degeneration (AMD)
- Dry macular degeneration is the most common form, and can be detected during a routine eye exam. It is considered the less aggressive form of AMD since it progresses slowly over many years or decades, and the clarity of vision slowly decreases over this time. It can result from aging and thinning of the macula, pigment in the macula, or a combination of the two causes.
- Dry AMD accounts for 80-90% of AMD cases.
-
- Wet macular degeneration is the more severe form of AMD. It usually develops rapidly as a result of abnormal blood vessel growth beneath the retina and leakage of blood and fluid, causing the development of blind spots and sudden loss of central vision.
If you suspect you have AMD, contact an eye doctor near you.
SEE RELATED: Macular Degeneration: Myths and Facts
Treatments for AMD
Although there is no cure for macular degeneration, there are treatments that can help to slow the advancement of the disease, preserve existing vision, and sometimes even improve vision loss.
How is dry AMD treated?
Treatment of dry AMD involves slowing the progression of the disease, using high doses of zinc and antioxidants.
The Age-Related Eye Disease Study (AREDS) shows that consumption of a specific formula of nutritional supplements containing high doses of antioxidants and zinc, may reduce AMD progression for those who have intermediate AMD, and those with advanced AMD in only one eye.
A follow up study known as AREDS2, importantly concluded that lutein and zeaxanthin should be substituted for beta-carotene. Lutein and zeaxanthin are also effective for maintenance of retinal health, while beta-carotene is associated with an increased risk of lung cancer in smokers.
With the results of AREDS2, it was proven that lutein and zeaxanthin reduced the risk of AMD progression by 19 percent, and of vision loss by 25 percent.
Currently, the AREDS and AREDS2 formulas are the only effective treatments for intermediate-to-severe dry AMD.
Dozens of “eye vitamins” and “ocular supplements” containing the special formula of nutrients have become widely available.
AREDS2 Formula
- 500 mg vitamin C
- 400 IU vitamin E
- 10 mg lutein
- 2 mg zeaxanthin
- 80 mg zinc
- 2 mg copper
How is wet AMD treated?
Treatment of wet AMD involves stopping the development of new blood vessels, destroying existing blood cells, and preventing leakage into the macula.
Treatment options for wet AMD include:
- Anti-VEGF treatment
- Laser surgery
- Photodynamic therapy
What is anti-VEGF treatment?
Vascular endothelial growth factor (VEGF) is a protein in your body that creates new blood vessels when your body needs them. If your body produces too much VEGF, abnormal blood vessels can grow in your eye. These abnormal blood vessels are dangerous to your eye health and vision— causing vision loss and even blindness.
Anti-VEGF treatments block the VEGF from creating new blood vessels to reduce vision loss, or inhibit further damage caused by the abnormal blood vessels.
The anti-VEGF medication is administered by your eye doctor. Your eye doctor will use an eye numbing agent to reduce pain during administration. A tiny needle will then be used to inject the medication into the white part of your eye (sclera)— this only takes a few seconds.
Your doctor will advise how many treatments will be necessary for treatment of your individual case.
How effective is the treatment?
- 9 in 10 people report stabilized vision
- 1 in 3 people report improved vision
Types of anti-VEGF medications
All of the medications have been proven safe and effective in the treatment of AMD. Each medication works to block the growth of abnormal blood vessels in the back of the eye, but differ in the type of drug they use, as well is their cost.
- Beovu uses a drug called aflibercep.
- Avastin uses a drug called bevacizumab.
- Lucentis uses a drug called ranibizumab.
- Eylea uses a drug called aflibercept.
- Mucugen uses a drug called pegaptanib sodium.
Laser photocoagulation
This laser surgery seals off the leaking abnormal blood vessels, while preserving healthy ones. This surgery will not restore any vision that has been lost, but can slow the progression of further vision loss.
Photodynamic therapy (PDT)
This treatment involves both a laser and a medicine called Visudyne dye, that is injected into a vein in your arm, and activated when exposed to light.
PDT is usually performed in an eye doctor’s office. Prior to the procedure, eye drops will be inserted into your eye to both dilate and numb your eye. After the Visudyne dye is injected, it travels through the bloodstream to the abnormal blood vessels under the retina. Using a special contact lens, your eye doctor will shine the laser into your eye, to activate the light-sensitive dye, causing it to seal off the abnormal blood vessels.
Post-procedure, your eye may be sore and your vision blurry— your eye doctor may cover your eye temporarily.
Additionally, you may be required to repeat this procedure, since the effects of the laser are often short-term.
Low vision devices
Although a treatment to fully regain vision loss from AMD has yet to be discovered, there are many low vision devices (i.e. magnifiers, telescopes, and other aids) that can facilitate your ability to maintain independence.
If you have been diagnosed with AMD, it is crucial that you continue to be monitored closely by your eye doctor.
Who is at risk for developing AMD?
Many times, in the early stages of macular degeneration, symptoms can go unnoticed. It is therefore crucial to have regular eye exams which can detect early signs of AMD— especially if you are at risk.
Many risk factors include:
- Age (over age 60)
- Family history
- Race
- Gender (female)
- Obesity
- High cholesterol
- Hypertension
- Smoking
- Exposure to ultraviolet (UV) rays
- Certain medications
How can you lower your risk of developing AMD?
Although there are risk factors that cannot be controlled, you can reduce your risk of developing AMD.
Schedule annual eye exams and inform your doctor of any family history of ocular disease.
- Avoid smoking
- Consume a healthy diet
- Get regular exercise
- Control cholesterol and blood pressure
- Wear 100% UV-blocking sunglasses
Take preventative measures to reduce your risk of developing AMD— this will not only help to preserve your ocular health, but your overall well being.
LEARN MORE: Guide to Eye Conditions
If you or a loved one may be experiencing symptoms of AMD, schedule an eye exam for a comprehensive evaluation.
If signs of AMD are detected, there are many effective treatments available to slow down or reduce vision loss, and many devices are available to support the existing vision.
Your eye doctor will discuss the most appropriate treatment and management options for you.