What is a macular disease?
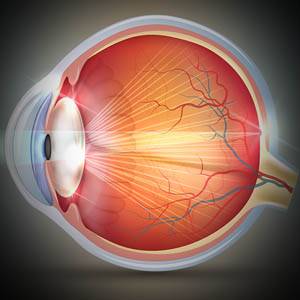
The macula is located in the center of the retina, and is responsible for enhancing our central vision with clear, sharp images. The macula also enables us to read fine print and notice small details
Macular disease occurs when the macular cells become damaged or destroyed, causing a gradual loss of central vision.
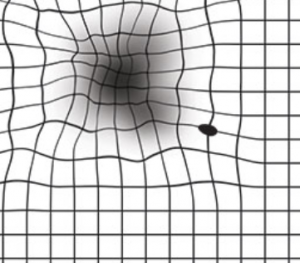
The best way to understand the effects of macular disease is to imagine taking a black marker and drawing all over the center of a photograph— preventing the ability to see faces, objects, and anything else that is right in front of you.
Common symptoms of macular disease include:
- Loss of central vision
- Loss of night vision
- Blurred or wavy vision
- Difficulty reading
- Loss of sharp color contrast
- Difficulty discerning colors
- Sensitivity to bright light
Different types of macular disease
Macular hole
A macular hole can occur when the macula tears or opens. This condition affects central vision, and can cause blurry, wavy, or distorted central vision. As the condition worsens and the hole becomes bigger, a dark blind spot will appear, blocking central vision.
A macular hole affects up to 4 in 1000 people aged 55 and older.
A macular hole can develop when the vitreous humor shrinks and pulls away from the retina— usually as a result of aging. In most cases, the vitreous can pull away from the retina without any complications. However, if the vitreous sticks to the retina, the macula begins to stretch and possibly tear, resulting in a macular hole.
In some cases, a macular hole can develop as a result of another eye disease that has caused the macula to swell. In other cases, a macular hole can occur from an eye injury or trauma to the retina.
Some macular holes may seal by themselves, but in most cases, a surgical procedure called a vitrectomy is used to treat the condition and improve vision.
Epiretinal membrane (macular pucker)
Epiretinal membranes (ERMs) are also known as cellophane maculopathy. When the ERM involves the macula, the condition is referred to as a macular pucker. Epiretinal membranes form on the inner surface of the retina, and resemble a wrinkled piece of cellophane. Overtime, the ERMs begin to contract and pull on the retina. When the ERMs affect the macula, they can cause visual distortions such as blurred or distorted vision, and vision loss.
Research has shown that ERM affects up to 2 percent of patients over age 50 and 20 percent over age 75.
The most common cause of ERM is posterior vitreous detachment (PVD), which occurs as the retina tears while being separated from the vitreous gel. Other causes include: diabetic retinopathy, CRVO or BRVO, eye trauma, eye surgery, or intraocular inflammation.
Treatment of this condition generally involves a surgical procedure called a vitrectomy.
If you experience symptoms of macular disease, contact an eye doctor near you.
SEE RELATED: What Is a Macular Hole?
Macular degeneration
Macular degeneration, also known as age-related macular degeneration (AMD), is an ocular disease caused by deterioration of the macula, the center of the retina that controls your visual acuity.
Macular degeneration accounts for 8.7% of all blindness worldwide, and is one of the leading causes of blindness in adults over the age of 60.
Macular degeneration causes dark “blind” spots to appear in the center of an image, or anything you are viewing, with gradual loss of central vision. There are two types of AMD:
- Dry macular degeneration is the most common form, accounting for 80-90 percent of AMD cases. Dry AMD can be detected during a routine eye exam. It is considered the less aggressive form of AMD since it progresses slowly over many years or decades, and the clarity of vision slowly decreases over this time. It can result from aging and thinning of the macula, pigment in the macula, or a combination of the two causes.
- Treatment of dry AMD involves slowing the progression of the disease, using high doses of zinc and antioxidants.
- Wet macular degeneration is the more severe form of AMD. It usually develops rapidly as a result of abnormal blood vessel growth beneath the retina and leakage of blood and fluid, causing the development of blind spots and sudden loss of central vision.
Treatment of wet AMD involves stopping the development of new blood vessels, destroying existing blood cells, and preventing leakage into the macula. This is typically accomplished through anti-VEGF injections, laser surgery, or photodynamic therapy.
Macular Telangiectasia
Macular Telangiectasia, commonly referred to as MacTel, occurs when the blood vessels that supply the macula become dilated and swollen around the fovea, which is located in the center of the macula and contains no blood vessels at all.
The actual cause of MacTel is poorly understood, but some suggest that it occurs as a result of a poor connection between the primary supporting cells of the retina, called muller cells, and the light-sensitive photoreceptor cells that enable central vision.
MacTel can lead to legal blindness, in which the patient experiences a significant loss of central vision, required for reading, writing, and driving. MacTel generally begins to develop in middle-aged patients, and gradually progresses over a period of 10 to 20 years.
There are two different types of MacTel, though both result in significant loss of central vision.
- Type 1 MacTel occurs when the swollen or dilated blood vessels (aneurysms) in the macula are localized. Aneurysms in the blood vessels cause the macular cells to swell, causing a disruption within the blood flow, and consequently causing bleeding and sometimes the development of fatty deposits.
- Type 2 MacTel, also called idiopathic juxta-foveal telangiectasia or idiopathic perifoveal telangiectasia, occurs for a reason that has yet to be discovered. However, Type 2 Mactel involves a more widespread dilation and leakage of damaged blood vessels— around the fovea of the macula.
Additionally, in Type 2 MacTel, new abnormal or fragile blood vessels begin to develop within the macula. However, due to their fragility, they subsequently leak blood and fluid— consequently causing scar tissue to form over the macula and fovea.
Symptoms of MacTel
Early symptoms of MacTel may be very subtle, so it is important to have regular eye exams to monitor your ocular health— especially if you are experiencing any of the following symptoms:
- Gradual loss of vision
- Distorted vision
- Difficulty reading
- Blindspot in visual field
Symptoms of MacTel may be stable for some time, with periodic sudden decreases in vision.
Patients who suffer from systemic conditions such as hypertension, diabetes, and coronary disease are at a higher risk of developing MacTel.
MacTel is a difficult condition to treat, as the progression of the disease is hard to control. In some cases, depending on the type of MacTel, anti-VEGF injections may be used. Many eye doctors recommend low vision assistive devices to improve the quality of life for those who have suffered vision loss. Your eye doctor will determine the most appropriate treatment plan for you.
LEARN MORE: Guide to Eye Conditions
If you have noticed any changes to your vision clarity, it is crucial to schedule a comprehensive eye exam for a thorough examination of your ocular health and vision.
Early detection of a macular disease can reduce the risk of severe vision loss, help to preserve remaining vision, and in some cases even improve vision that has been affected by the disease.