Corneal conditions can permantly impact your vision.
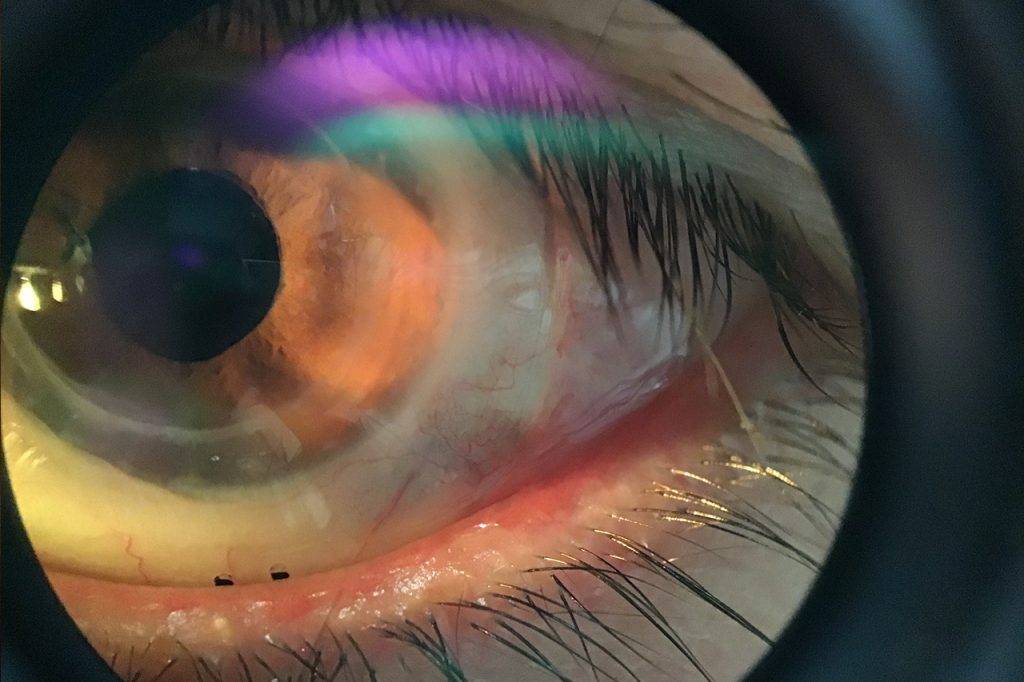
The cornea is the clear, protective outer layer of the eye. It’s primary function is to act as a barrier and filter for the eye— preventing harmful particles from penetrating the eye, and filtering out the sun’s ultraviolet rays.
What is the primary function of the cornea?
The cornea plays an essential role in your vision.
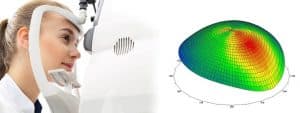
As light enters the eye, it first reaches the cornea, the clear dome-like structure at the front of the eye. At At the cornea, the light is refracted, or bent, according to the shape of the cornea. The curvature, or shape of the cornea, determines the eye’s focusing abilities of the eyes.
What are corneal dystrophies?
Corneal dystrophies are diseases that cause structural problems within the cornea. More than 20 types of corneal dystrophies have been discovered.
The most common corneal dystrophies include:
1. Keratoconus
Keratoconus is a progressive disease that causes thinning and reshaping of the cornea. A distorted shape of the cornea, similar to a cone, leads to vision changes— usually a mild to severe astigmatism, and nearsightedness. Keratoconus can also cause corneal swelling and scarring, and even vision loss.
Keratoconus is often diagnosed among teens and young adults, and progresses for up to 20 years until it plateaus.
Symptoms of keratoconus;
- Light sensitivity
- Glare
- Irritation
- Vision changes
Causes of keratoconus
- Genetics
- Eye trauma
- Other eye diseases
- Down syndrome
- Osteogenesis imperfecta
- Addison’s disease
- Leber’s congenital amaurosis
- Ehlers-Danlos Syndrome
Keratoconus treatment
1) Eyeglasses and contact lenses
In its early stages, the condition can be corrected with eyeglasses or soft contact lenses.
As the disease progresses, rigid gas permeable contact lenses may be required for adequate correction.
2) Intacs surgery
Intacs are thin plastic, semi-circular rings that are inserted into the middle layer of the cornea to flatten the cornea— changing the shape and location of the cone. The intacs reinforce the cornea and eliminate the abnormalities caused by keratoconus, to facilitate improved vision.
This procedure can improve vision without the need for corrective eyewear. However, in severe cases, glasses or contact lenses may still be required.
3) Corneal transplantation
In advanced keratoconus, a corneal transplant may be necessary to replace the damaged cornea with a new one. This surgery is successful in about 9 out of 10 people. Eyeglasses or contact lenses will most likely be required even after the transplant.
4) Corneal cross-linking
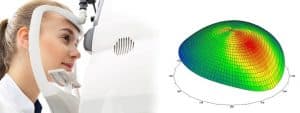
Corneal cross-linking is an in-office procedure used to strengthen the cornea if it’s been affected by keratoconus, other corneal disease or, in rare cases, as a complication of LASIK surgery.
During the procedure, the front layer of the cornea is removed, and an eye drop of liquid riboflavin (vitamin B2) is applied to the surface of the eye. Ultraviolet light (UV) is then administered to the eye at varying levels of time and intensity, and is absorbed by the cornea. The UV light functions to stabilize the cornea and slow the progression of disease.
The procedure takes around 90 minutes to perform.
When corneal cross-linking is used in the early stages of keratoconus, it can prevent vision loss even before corrective lenses are needed— this highlights the importance of an early diagnosis!
If you suspect you have an eye condition, contact an eye doctor near you, who can diagnose and treat the condition.
SEE RELATED: Keratoconus
2. Map-Dot-Fingerprint dystrophy
Map-dot-fingerprint dystrophy causes abnormal folds and reduplications of the epithelium layer of the cornea, creating patterns that resemble maps, dots, and small fingerprints.
This condition usually affects adults ages 40 to 70. It may also affect children, if inherited. It is usually painless and typically does not cause vision loss.
In some cases however, epithelial erosions may occur— exposing the lining of nerves of the cornea, and causing intense pain, in addition to astigmatism and nearsightedness.
Symptoms of map-dot-fingerprint dystrophy
- Pain
- Blurry vision
- Sensitivity to light
- Excessive tearing
- Foreign body sensation
Treatment map-dot-fingerprint dystrophy
In most cases, treatment is not required.
However, if epithelial erosions occur, your eye doctor may prescribe lubricating ointments, special contact lenses, or a minor surgical procedure to debride the abnormal tissue on the surface of the eye.
3. Fuch’s dystrophy
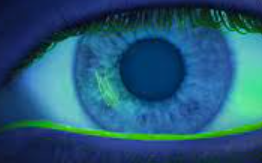
Fuch’s dystrophy is a gradual deterioration of the corneal endothelium, or innermost layer of the cornea, that causes the cornea to swell— resulting in blurred vision.
Some patients with Fuch’s dystrophy complain of blurred vision in the morning that slowly clears up as the day progresses.
As the disease progresses, swelling becomes more consistent— causing blurry vision at all times.
In the advanced stages of this disease, small blisters may appear on the corneal surface, causing pain and irritation.
Symptoms of Fuch’s dystrophy generally begin to present in patients ages 30 to 40 years— though vision usually remains unaffected until about 20 years later. It is more common in women than men.
Treatment for Fuch’s dystrophy
Ointments and eye drops may be prescribed for mild symptoms. For significant vision impairment and chronic pain associated with the disease, a corneal transplant may be recommended.
4. Lattice dystrophy
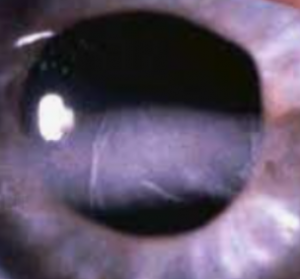
Lattice dystrophy occurs with the presence of abnormal protein fibers throughout the stroma. While this condition can develop at any age, early signs of the disease can be identified in childhood.
Lattice dystrophy has earned its name from the clear overlapping lines of proteins that create a lattice design in the stroma. This can cause cloudy and reduce vision. In some patients, these proteins may cause epithelial erosion.
Treatment of lattice dystrophy
Your eye doctor may prescribe eye drops or ointment for symptomatic irritation to alleviate symptoms. For severe vision loss or chronic pain associated with the disease, a corneal transplant may be recommended.
LEARN MORE: Guide to Eye Conditions
If you are experiencing any ocular pain or discomfort, or have noticed any vision changes, schedule an eye exam as soon as possible.
With proper diagnostic tools and assessments, your eye doctor can detect signs of corneal dystrophy, or any other ocular disease, even in its early stages— and will provide an effective treatment plan to alleviate your symptoms and reduce your risk of vision loss.