Over 1 in 4 of all people with diabetes develop macula edema within 10 years of their diagnosis.
What is diabetic macular edema (DME)?
Diabetic macular edema (DME) is a complication that can result from a diabetic ocular disease, called diabetic retinopathy.
- Diabetic macular edema is the most common cause of vision loss in people with diabetic retinopathy.
- Approximately 7.7 million Americans suffer from diabetic retinopathy, among those people, about 750,000 also have DME.
- 6.8% of people with diabetes have DME
- Up to 25% of people with diabetes develop DME within 10 years of their first diagnosis.
What is diabetic retinopathy?
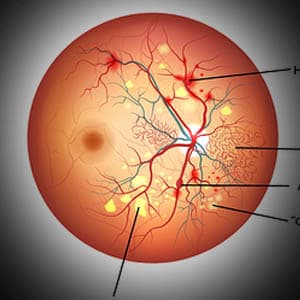
Diabetic retinopathy affects people with diabetes, and occurs when high levels of sugar in the bloodstream cause progressive damage to the retina.
Diabetes causes damage to the blood vessels in the body, including the retina. As a result, the blood vessels leak blood and other fluid into the eye, causing the retinal tissue to swell— and cloudy or blurred vision. Moreover, as these blood vessels are destroyed, new abnormal blood vessels are produced. These new blood vessels are fragile and even more susceptible to leaking and bleeding fluid into the eye.
Diabetic macular edema occurs when damaged blood vessels from the retina leak fluid into the macula, the center of the retina.
Diabetic macular edema can occur at any stage of diabetic retinopathy, though it generally develops as the disease progresses to more advanced stages.
Diabetic macular edema causes the macula to swell and thicken, resulting in distorted vision.
Other causes of DME
While DME is most commonly caused by diabetic retinopathy, it may also occur after eye surgery, from age-related macular degeneration, an inflammatory eye disease, or high blood pressure.
People with DME are at a higher risk of permanent vision loss if they have poorly controlled blood sugar levels, or any other medical conditions such as high blood pressure.
Symptoms of DME
Diabetic macular edema may range from mild blurry vision to significant vision loss, and can affect one or both eyes.
Common symptoms include:
- Blurry or wavy vision
- Blind spots
- Colors appear dull
- Difficulty reading
- Trouble with facial recognition
- Difficulty driving
If only one eye is affected, blurry vision may not be noticed until the disease is more advanced.
Types of DME
There are two different types of DME. With a comprehensive eye exam, your eye doctor will determine which type is affecting your vision. Diabetic macular edema can be classified based on:
- The amount of retinal swelling present— increased swelling causes greater vision loss.
- The location of damage to the blood vessels— localized or widespread.
How is DME diagnosed?
Your eye doctor may utilize any of the following diagnostic tools to determine the presence of DME:
Optical coherence tomography (OCT) to measure the amount of retinal swelling. The OCT scan uses a laser, without radiation, to obtain higher resolution, color-coded images of the layers of the retina and optic nerve.
Fundus imaging to capture detailed images of the retina, for detection of irregular blood vessels.
Fluorescein angiography to highlight the blood flow in the retina, for identification of abnormalities. This test involves the use of a special dye that is injected into a vein in the arm, and travels to the retina where it is illuminated.
If you have diabetes, contact an eye doctor near you, who can diagnose and discuss the best treatment options.
SEE RELATED: Why Does Diabetes Cause Blurry Vision?
How is DME treated?
The treatment your eye doctor will recommend, will be dependent on the type of DME you have been diagnosed with. In some cases, more than one type of treatment will be required.
1. Controlling blood sugar levels
Before treating the DME, the underlying cause needs to be addressed and controlled. In most cases, the macula is affected by the high levels of sugar in the bloodstream. This means that active steps need to be taken in order to control your blood sugar levels.
Speak to your primary care physician about effective ways to control your diabetes.
2. Anti-VEGF injections
There is a protein in your body called VEGF. In normal amounts, this protein is responsible for aiding in the creation of new blood cells. However, if you have DME, your body is making too much VEGF, causing the blood vessels to grow too quickly— making them more prone to breaking and leaking blood and fluid into your retina and macula.
Anti-VEGF medications are injected directly into the center of the eye with a thin needle, to block the overproduction of the VEGF protein.
There are three anti-VEGF medications used for DME:
- Aflibercept (Eylea)
- Bevacizumab (Avastin)
- Ranibizumab (Lucentis)
What should I expect with anti-VEGF injections?
Your eye doctor will first numb your eye, before injecting the medication, so you shouldn’t feel any pain. The medication will need to be re-administered every month, for the first six months. Your doctor will then advise when to come back for another dose of medication— slowly weaning you off of the medication over the next few years.
You will notice that your vision has recovered once your blood vessels have stopped leaking, as a result of the medication.
Anti-VEGF may not be effective for everyone. In this case, your eye doctor may recommend focal-grid macular laser surgery.
3. Focal-grid macular laser surgery
Laser surgery is another effective treatment method for DME. This surgery involves sealing the leaking blood vessels to decrease swelling.
Focal-grid laser surgery will be performed on one eye at a time. If you have DME in both eyes, your eye doctor will advise when to schedule a second surgical procedure, usually a few weeks after the first procedure.
In most cases, one laser surgery will be effective in treating DME, and multiple procedures will not be necessary.
4. Corticosteroids
Corticosteroids are prescribed to reduce inflammation, and in this case the swelling in your retina.
Steroids may be directly injected into your eye, or sometimes even implanted into your eye. A steroidal implant is placed in the eye with a special device, and works by slowly releasing small doses of medicine overtime. The implant also dissolves into your bloodstream, eliminating the need to have it taken out.
Steroids are generally used as a last resort, if other treatments have failed to be effective. This is because they typically don’t work as well as anti-VEGF medications, and can also pose a risk to your ocular health— increasing your chances of developing cataracts and glaucoma.
5. NSAID eye drops
Nonsteroidal anti-inflammatory drugs (NSAIDs) help to reduce inflammation, but do not contain the same side effects as steroids. Your eye doctor might recommend NSAID eye drops to help reduce retinal swelling, before or after DME surgery.
If untreated, diabetic macular edema can cause vision distortions and even permanent vision loss.
LEARN MORE: Guide to Eye Conditions
If you have diabetes and experience any changes in your vision, schedule an eye exam as soon as possible.
An early diagnosis and effective treatment plan will prevent further vision loss from DME, and may even help to recover lost vision.